HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
In This Section
How Can We Improve Nurse Response Times to Bedside Alarms?

The findings:
When it comes to bedside alarms for conditions like low oxygen saturation, tachycardia, or cardiac arrhythmias, four main factors contribute to faster nurse response times:
- Nurses responded faster to patients on complex care service and those without family members at their side.
- Nurses responded faster if they had less than 1 year of experience, had a 1 to 1 assignment, or had previously responded to the same patient’s alarm.
- Nurses responded fastest to lethal arrhythmia alarms.
- For each hour that passed in a nurse’s shift, response time got a little bit slower.
When the researchers looked only at actionable alarms (these are the important ones we would not want anyone to miss), the average response time was very fast: under one minute.
Why it matters:
Bedside monitor alarms help hospitalized children get immediate attention for life-threatening physiologic changes. However, the current response times of nurses may be slow – clocking in at an average of seven minutes – despite the potential urgency of some alarm situations. If researchers can identify the specific factors that contribute to fast or slow response times, we can work to improve or optimize them for serious situations.
Who conducted the study:
Researchers from the division of General Pediatrics, Clinical Futures, a CHOP Research Institute Center of Emphasis, department of Anesthesiology and Critical Care Medicine, and department of Nursing at Children’s Hospital of Philadelphia; researchers from the Leonard Davis Institute of Health Economics and Department of Biostatistics and Epidemiology at the University of Pennsylvania’s Perelman School of Medicine; and one researcher from the Touro College of Osteopathic Medicine.
How they did it:
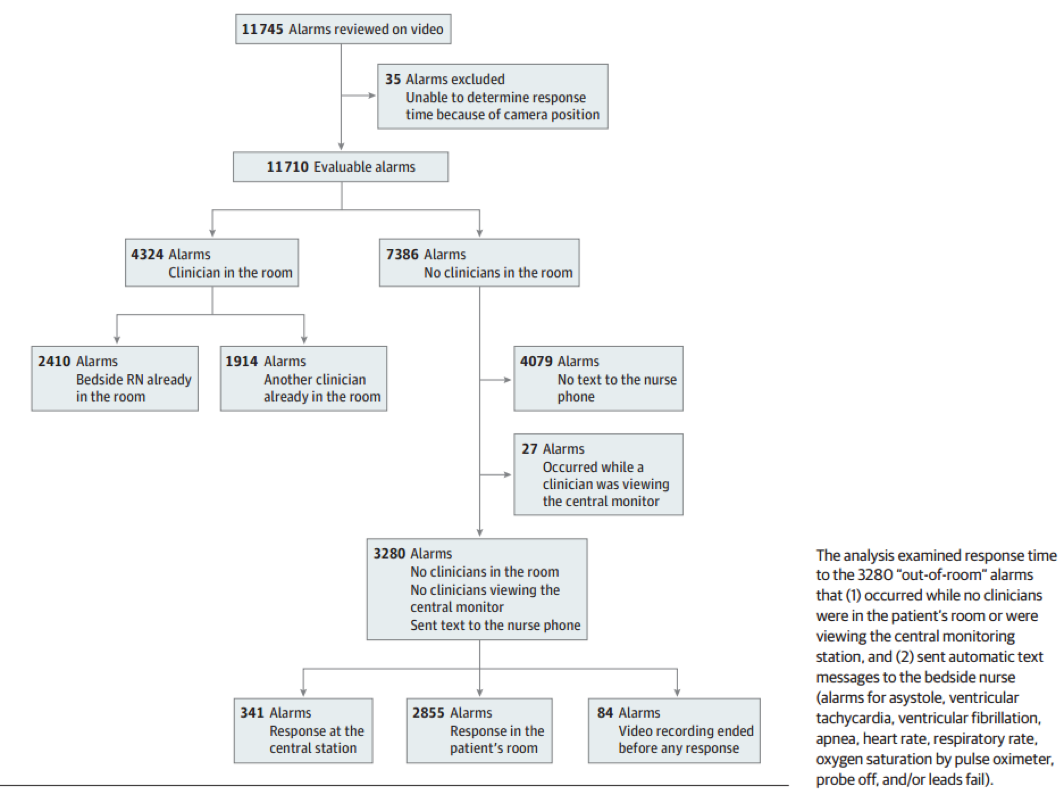
The researchers analyzed 100 video recordings of 100 patients and 38 nurses over 551 hours in one inpatient unit at Children’s Hospital of Philadelphia, and they combined that video with time-stamped alarm data from the monitoring network. The study team used multivariable accelerated failure-time models to evaluate the potential link between certain risk factors and response time while the nurse was outside the room.
Source: JAMA Pediatrics
What’s next:
According to Christopher Bonafide, MD, attending physician at CHOP and the study’s first author, the researchers are working with collaborators at several different institutions to design and test a number of different approaches to reduce unnecessary alarms so that when alarms go off, they are much more meaningful and prompt nurses and other clinical staff to take action. The quick response to actionable alarms (under one minute) from the current study suggests that the nurses were highly skilled at predicting which alarms were going to be important.
Where the study was published:
Who helped fund the study:
The National Heart, Lung, and Blood Institute of the National Institutes of Health helped fund the study through a Mentored Patient-Oriented Research Career Development Award.
Where to learn more about the study:
You can find the study online at JAMA Pediatrics, and also learn more about the paper’s first author Dr. Christopher P. Bonafide, MD’s novel use of videos to understand alarm fatigue on Cornerstone.