HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
In This Section
What Affects How Nanoparticles Interact With Our Immune System?
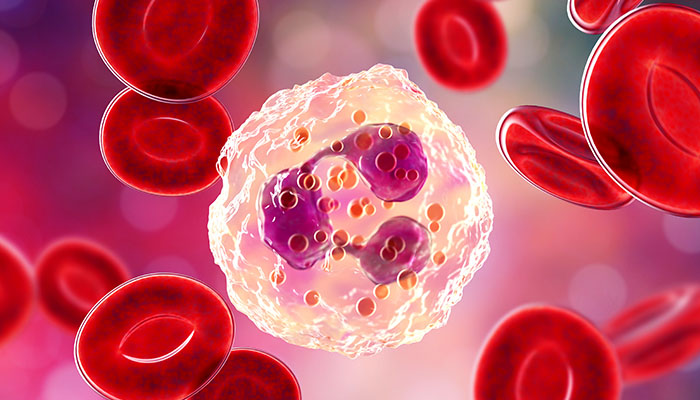
Researchers described the mechanism behind how nanoparticles interact with neutrophils in a recent Nature Nanotechnology paper.
limjr [at] chop.edu (By Jillian Rose Lim)
The findings:
Researchers at Children's Hospital of Philadelphia have elucidated how the organization of nanoparticle surface proteins affect how particles interact with "first-responder" immune cells called neutrophils. In a new study, Kathryn Rubey, MD, attending physician in our Division of Neonatology, and her colleagues described their novel discovery of the nanomaterial property that dictates this interaction. Nanoparticles evade the immune system when their surface proteins are regularly organized. But when proteins are arranged in a random assortment, neutrophils can recognize and engulf the particles.
Why it matters:
The findings have important translational significance for treating a wide range of diseases. Now that researchers understand the mechanism dictating neutrophil-nanoparticle interactions, particles can be designed to target or evade immune cells, depending on the disease mechanism. For example, Dr. Rubey and colleagues are currently applying this technology to lung diseases that are heavily mediated by the patient's immune response: pneumonia, caused by bacterial and viral infections, and acute respiratory distress syndrome (ARDS), an inflammatory lung condition causing acute respiratory failure. Dr. Rubey and her colleagues are studying how the design of nanoparticles might deliver antibiotics to the lungs, or modulate the pulmonary immune response to reduce damage caused by inflammation, respectively, in these conditions.
Who conducted the study:
Dr. Rubey, a first author of the paper, conducted the research with a multi-institute team.
How they did it:
While many researchers seek to add things to nanoparticles to direct particle delivery to specific body sites, Dr. Rubey's team went about their work in a different way: The researchers discovered a property wherein no additions are necessary to direct nanoparticles to the lungs. They then defined the mechanism behind that property and discovered that it targets immune cells, called neutrophils, which are involved in the body's response to inflammation or infection.
Quick thoughts:
"There's a variety of ways that we'll be able to both design and load these particles with a range of pharmaceuticals to treat different diseases," Dr. Rubey said. "Innovation in rational antibiotic use and targeted antibiotic delivery is so important right now, as we continue to have more and more antibiotic resistance. While we are thoughtful about appropriate antibiotic use and avoid over-use, antibiotics remain a critical tool in the treatment of life-threatening infections. Unfortunately, there's not a lot of innovation happening currently in terms of new antibiotic drugs, so we need to avoid building resistance against the drugs we do have available. The goal is if we change the mode of drug delivery, we could change the way we use antibiotics and the side effects we encounter — potentially directly treating pathogenic bacteria while saving the microbiome, or good bacteria."
What's next:
Dr. Rubey said next steps include further investigation of antibiotic delivery using nanoparticles. For example, she will investigate whether delivering antibiotic-loaded nanoparticles will improve neutrophils' clearance of pneumonia.
Where the study was published:
The study "Supramolecular arrangement of protein in nanoparticle structures predicts nanoparticle tropism for neutrophils in acute lung inflammation"appeared online in Nature Nanotechnology.


