HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
In This Section
Exploring the Wide World of the Microbiome
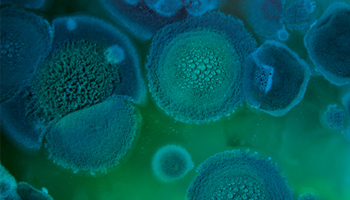 Studying the microbiome — the 40 trillion or so invisible microbes that call your body home — is like being an explorer of a secret world with its own language and lifeforms. Whether these microbes are sometimes friends or sometimes foe depends on subtle interactions with each other and the role of influential factors such as your genetics, environment, age, and diet.
Studying the microbiome — the 40 trillion or so invisible microbes that call your body home — is like being an explorer of a secret world with its own language and lifeforms. Whether these microbes are sometimes friends or sometimes foe depends on subtle interactions with each other and the role of influential factors such as your genetics, environment, age, and diet.
The PennCHOP Microbiome Program awards annual pilot and feasibility grants to help faculty members of the University of Pennsylvania and Children’s Hospital of Philadelphia scientific communities navigate this uncharted territory. With the funding awarded in 2017, eight projects are underway, and CHOP clinician-scientists are leading two of them.
Leveraging the Immune System for Effective Protection
 Michael Silverman, MD, PhD, a physician within the Division of Infectious Diseases at CHOP and an assistant professor of Pediatrics at Penn, is leveraging the immune system to mine for microbes that prevent autoimmune disease, which occurs when the body’s immune system attacks its own healthy cells and tissues. In this pilot study, Dr. Silverman is focusing on Type 1 diabetes, a chronic autoimmune disease that causes the pancreas to produce little or no insulin. Without insulin, sugar builds up in the bloodstream, and if left untreated, the excess sugar in the blood can cause severe damage to the body.
Michael Silverman, MD, PhD, a physician within the Division of Infectious Diseases at CHOP and an assistant professor of Pediatrics at Penn, is leveraging the immune system to mine for microbes that prevent autoimmune disease, which occurs when the body’s immune system attacks its own healthy cells and tissues. In this pilot study, Dr. Silverman is focusing on Type 1 diabetes, a chronic autoimmune disease that causes the pancreas to produce little or no insulin. Without insulin, sugar builds up in the bloodstream, and if left untreated, the excess sugar in the blood can cause severe damage to the body.
Some people have a strong genetic component within the human leukocyte antigen (HLA) region of the genome that increases their risk for getting Type 1 diabetes. Yet, it appears that other people inherit versions of HLA genes that gives them dominant protection from the disease. Dr. Silverman is working with mouse models to better understand how that protective process works.
“What we’ve figured out is that the gene protects by modulating, or controlling, the development of the microbiome to give you protective microbes,” Dr. Silverman said. “And then those protective microbes talk back to the immune system and push it away from autoimmunity.”
One of the key questions that this pilot grant is trying to answer is: What are the immunomodulatory microbes — those that change how the immune system develops or functions — that are protective? That is a challenging question because scientists must narrow down which are the most important microbes involved in this process from about 1,000 types that fluctuate in your gut.
Dr. Silverman relies on antibody response — when the immune system makes a specific antibody against a particular microbe in the gut — as a signal to direct his search. First, he isolates the antibodies appearing in a mouse model that is protected from Type 1 diabetes. Next, he determines which microbes those antibodies recognized. And then he uses flow cytometry technology to pull out each of those microbes tagged by an antibody, sorts them, extracts their DNA, and identifies each type of microbe that could help to shape the immune system away from autoimmunity.
An insight that Dr. Silverman has gained from the pilot project so far is that the immunomodulatory communication between the immune system and the gut microbiota seems to take place very early in life, right around the time the mice wean. This suggests that any potential therapeutic interventions for humans likely would be most valuable during infancy or early childhood, and they could have profound and long-term impacts on the immune system and overall health.
“I think there is this time window early in life when your microbes really teach your immune system how to behave,” Dr. Silverman said. “If we can find the right microbes to teach the immune system to behave properly, and not develop autoimmunity, that’s the translational potential.”
Role of Host-Microbiota Interactions in Inflammation
 As part of his pilot study project, Lehn Weaver, MD, PhD, a physician within the Division of Rheumatology at CHOP and an instructor of Pediatrics at Penn, is looking for early inflammatory cues influenced by the microbiome that could contribute to the development of pediatric rheumatic diseases such as systemic juvenile idiopathic arthritis (SJIA). Children with this type of autoimmune develop arthritis, rash, daily fevers, and inflammation of internal organs.
As part of his pilot study project, Lehn Weaver, MD, PhD, a physician within the Division of Rheumatology at CHOP and an instructor of Pediatrics at Penn, is looking for early inflammatory cues influenced by the microbiome that could contribute to the development of pediatric rheumatic diseases such as systemic juvenile idiopathic arthritis (SJIA). Children with this type of autoimmune develop arthritis, rash, daily fevers, and inflammation of internal organs.
Based on his experiences seeing SJIA patients in the clinic, Dr. Weaver has observed that about 10 percent to 30 percent of the patients with SJIA appear to have an underlying predisposition to develop macrophage activation syndrome (MAS). Also known as a cytokine storm syndrome, MAS occurs when the body’s immune system rages out of control, resulting in overwhelming inflammation, rapid organ failure, and death, if not quickly diagnosed and treated.
“We are very interested in trying to figure out which patients are most at risk for developing MAS because they oftentimes become some of the sickest patients in the hospital,” Dr. Weaver said.
Dr. Weaver’s investigations are based on a mouse model of MAS. The goal of his pilot project is to identify individual microbes and microbial-derived products that correlate with the mice’s susceptibility to over-inflammation. Once he is able to point to which microbes are likely troublemakers involved in promoting the MAS inflammatory cascade, then scientists can perform further studies to see if this microbial signature is helpful in predicting which patients are predisposed to MAS.
“Our findings so far indicate that to develop MAS, you need two different signals that lead to the amplification of the inflammatory response: an inflammatory signal from systemic juvenile arthritis and an inflammatory signal from the host microbiota,” Dr. Weaver said.
Both Drs. Silverman and Weaver said they were grateful for the funds, guidance, and technical and analytical expertise provided by the PennCHOP Microbiome Program. The pilot grants allowed them to get their projects underway seamlessly, move the science forward, and lay the groundwork for future investigations to identify host-microbiota interactions that could be targeted for therapeutic benefit.
Submissions for the next round of pilot grants are due by 5 p.m. EST March 16, 2018. For more information, visit the PennCHOP Microbiome Program website. Awards will be announced in June 2018.