HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
In This Section
Collaborative Discovery Supports Next Wave of Pediatric Brain Tumor Innovation
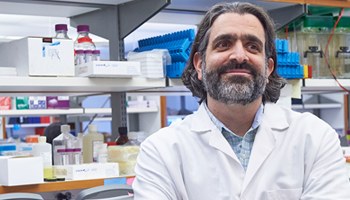 Editor’s Note: Childhood brain tumors remain some of the most difficult to treat cancers, especially because of current therapies’ long-term side effects for the survivors. In honor of Brain Tumor Awareness Month, Adam Resnick, PhD, director of the Center for Data-Driven Discovery in Biomedicine (D3b) at Children’s Hospital of Philadelphia, is our guest blogger. He brings us up to date on how the CHOP-led consortia, working with patients, families, and partnering institutions, has witnessed first-in-kind initiatives and innovative clinical trials aimed at personalized, precision-based approaches for brain tumors that are redefining the scientific landscape of research and therapeutic translation.
Editor’s Note: Childhood brain tumors remain some of the most difficult to treat cancers, especially because of current therapies’ long-term side effects for the survivors. In honor of Brain Tumor Awareness Month, Adam Resnick, PhD, director of the Center for Data-Driven Discovery in Biomedicine (D3b) at Children’s Hospital of Philadelphia, is our guest blogger. He brings us up to date on how the CHOP-led consortia, working with patients, families, and partnering institutions, has witnessed first-in-kind initiatives and innovative clinical trials aimed at personalized, precision-based approaches for brain tumors that are redefining the scientific landscape of research and therapeutic translation.
While CHOP’s Neurosurgical and Neuro-Oncology clinics are renowned leaders in treating and caring for children diagnosed with brain tumors, collecting sufficient numbers of tumor samples for an empowered, comprehensive molecular analysis that could lead us to new and better treatment approaches would take decades at a single institution. This was the impetus for the 2011 launch of the Children’s Brain Tumor Tissue Consortium (CBTTC) at CHOP, and it has gained momentum with nearly 50 scientific projects supported to date.
The CBTTC began with four partnering institutions seeking to define the molecular underpinnings of pediatric brain tumors through a shared biorepository collecting tumor biopsies and deep, longitudinal data. Through engaged collaboration, the CBTTC has grown exponentially in both the number of specimens collected and partnering institutions. To illustrate this phenomenal growth, in May the CHOP Research Institute hosted the 4th International CBTTC Investigator meeting, with attendees representing more than 18 national and international institutions.
 Later this year, we will mark a milestone with the landmark release of the largest molecular and genomic open pediatric brain tumor dataset of its kind. The release represents the first large-scale whole genome sequencing of childhood cancers. Not only is the size of the dataset of importance, but also the way it will be shared with other investigators around the world. The data from this study will be available to the research community via cloud-based infrastructures that empower rapid access, shared discovery, and accelerated analysis. With more than 2,000 patients enrolled in the CBTTC across more than 50 different brain tumor diagnoses, the genomic and gene expression datasets will also provide the foundation for a planned Childhood Brain Tumor Atlas, in which we aim to characterize the clinical, imaging, cellular, proteomic, and genomic features of these tumors in ways that can be translated to novel clinical therapies and targeted approaches.
Later this year, we will mark a milestone with the landmark release of the largest molecular and genomic open pediatric brain tumor dataset of its kind. The release represents the first large-scale whole genome sequencing of childhood cancers. Not only is the size of the dataset of importance, but also the way it will be shared with other investigators around the world. The data from this study will be available to the research community via cloud-based infrastructures that empower rapid access, shared discovery, and accelerated analysis. With more than 2,000 patients enrolled in the CBTTC across more than 50 different brain tumor diagnoses, the genomic and gene expression datasets will also provide the foundation for a planned Childhood Brain Tumor Atlas, in which we aim to characterize the clinical, imaging, cellular, proteomic, and genomic features of these tumors in ways that can be translated to novel clinical therapies and targeted approaches.
These are exciting times for CBTTC, and we are fortunate to have some of the most innovative minds working with us every step of the way. Housed within the D3b, I lead the CBTTC Coordinating Center along with Phillip Storm, MD, in Neurosurgery; Angela Waanders, MD, in Neuro-Oncology; and their partners in Pathology, including Mariarita Santi, MD, PhD, and Marilyn Li, MD. The Coordinating Center role of CHOP is supported by a transdisciplinary team encompassing multiple clinical divisions, departments, as well as Research Institute cores and partners at CHOP, including the Biorepository Core.
And our efforts extend beyond the CHOP campus and our resident experts. Partnering with the CBTTC and empowering the scientific translation of large-scale genomic data to clinical trials is the Pacific Pediatric Neuro-Oncology Consortium (PNOC), a clinical trial consortium initially launched in California with sites now across the United States. CHOP leads the data coordination and integration efforts of PNOC, and I serve as its Scientific Chair.
This past year, PNOC launched clinical trials focused on novel precision-based approaches for some of the most devastating of brain tumors, including diffuse intrinsic pontine gliomas (DIPG). With no successful therapies defined for DIPG after more than 50 years of research, PNOC embarked on a molecularly guided clinical trial. For the first time, patients underwent clinical biopsies of their tumors with the samples rapidly undergoing a comprehensive genomic and gene expression analysis that can be informed by the large-scale curated genomic datasets. Partnering with the Translational Genomics Research Institute (TGen), a panel of clinical experts defined up to four drugs that could be combined to specifically target the altered pathways in an individual patient’s tumor, providing for a personalized therapeutic approach for each child in the trial.
Together with its partners, CHOP’s consortia-based efforts in pediatric brain tumors represent vanguard initiatives that seek to transform the care of patients and the timescales by which research is translated to the clinical setting. The efforts have grown rapidly, and over the coming years will represent one of the largest national initiatives on behalf of pediatrics via the Kids First Data Resource Center (Kids First DRC), a newly launched, NIH-sponsored 10-year initiative that will support the sequencing by the end of 2018 of more than 25,000 genomes of children affected by cancer and structural birth defects. The Kids First DRC seeks to transform our understanding of childhood disease via the very same principle originally defined by the CBTTC — rampant collaboration and data sharing with patients as partners. The Kids First DRC will support the next wave of brain tumor innovation, as collaborative discovery expands across the childhood disease discovery ecosystem, connecting patients, families, researchers and clinicians on behalf of a shared goal of accelerated discovery.


