HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
In This Section
Centralized Model Key to Genomic Testing, Treatment, and Management
Building a community, adaptability, teamwork, and flexibility are central to the RIGMC’s accomplishments.
By Nancy McCann
Athan just turned 1-year-old, and he keeps his parents, Kristen and John Fullam, on their toes, literally.
“He crawls so fast, we need to run after him to keep up — and he just started walking last week,” Kristen said with a smile. Hitting his developmental milestones, Athan’s first words were “baba,” yum,” and much to mom’s delight, “mama.”
“This is the same baby who was in the NICU for the first three months of his life and, at one point, we were told he may not make it,” Kristen said. “He is the baby who had 16 different departments in the hospital trying to figure out what was wrong.”
As his doctors worked frantically to find answers to his challenging condition, Athan remained in the NICU receiving blood platelet transfusions three times-a-day, while his parents endured repeated disappointments as the tests ordered continued to return negative results.

Athan Fullam on his first birthday.
“We made sure we were present during rounds each morning to hear how Athan was doing and continue to learn what was happening to him medically,” Kristen said. “We learned how to read the monitors Athan was hooked up to, and so much more. We would write down lists of questions to ask doctors every morning during rounds. We wanted answers and would try anything to try to find them.”
The diagnostic break finally came after Athan’s doctors referred the family for genomic testing at CHOP’s Roberts Individualized Medical Genetics Center (RIGMC). Through this test, Athan was found to have NLRC4-MAS, a novel, primary autoinflamatory syndrome caused by mutations in the NLRC4 gene. He is only the 21st patient to be identified with this rare, life-threatening condition — and the youngest.
Athan’s story is one of the successes of the RIGMC model reported this week in Pediatrics by co-authors physician-scientist Ian Krantz, MD, and senior genetic counselor Livija Medne, MS, LCGC. The journal article provides a working blueprint for other hospital systems to facilitate access to state-of-the-art individualized genetic and genomic testing and management for children and families, just like the Fullam’s.
“The RIMGC is the first-of-its-type built in a focused way in the country in a pediatric setting,” said Dr. Krantz, director of the Center and a professor of genetics at the Perelman School of Medicine at the University of Pennsylvania. “Centralizing it allowed us to develop the expertise, not only to navigate this whole process and to work closely with the Division of Genomic Diagnostics (DGD), but also to become familiar with the genetic causes of isolated pediatric conditions that were not traditionally referred to and seen in genetics.”
Study Provides Model of Centralized Approach
Recognizing that next generation gene sequencing (NGS) has the ability to revolutionize the diagnostic process by allowing for the development of highly targeted therapies and more nuanced treatment strategies, CHOP opened the doors of the Roberts Individualized Medical Genetics Center in 2014 as the first pediatric individualized genomic program in the country.
The Center is part of the Division of Human Genetics and provides interpretative and educational support to clinicians pursuing this testing for their patients. These unique services rely on the expertise of RIMGC’s team of physicians, genetic counselors, research coordinators, bioinformaticians, laboratory technicians, and administrators.
“Since the Center opened, we have seen how the demand for genetic and genomic services will require a different approach beyond what traditional divisions and departments specializing in this field are able to provide,” said Dr. Medne, co-director of the Center. “Our experience shows how a model like this allows for those growing needs to be properly met and sufficiently supported.”
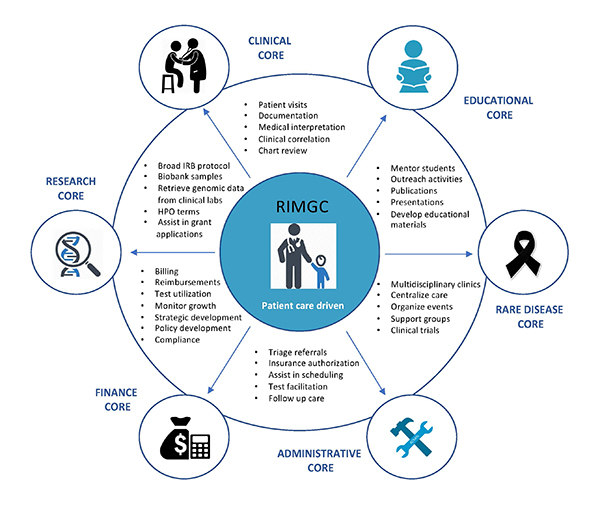
The RIMGC centralized model — a blueprint for other hospital systems.
And it’s here, where this team of experts, working with Athan’s physicians, including chief of the Division of Rheumatology, Edward Behrens, MD, diagnosed his extremely rare condition after performing complete exome sequencing that allows for analysis of all of our 20,000 genes in a single test. Athan began a clinical trial medication the next day, after which they started to see a huge turn in his clinical labs and his appearance.
“We celebrated the day we were told Athan didn’t need a platelet transfusion; he ended up having approximately 35 platelet transfusions during his three-month stay,” Kristen said.
On May 21, the Fullam’s were released from the hospital. Kristen and John took Athan home and have not been readmitted again for his NLRC4-MAS condition.
“If it was not for RIMGC, we would not have been able to start the clinical trial as soon as we did,” Athan’s mom enthused. “We were so lucky to be in a hospital that has a genetic center and works so closely with all departments of the hospital.”
The Age of Genomics is Here
As genomic testing continues to expand and reach all specialties and medical practices, increasing support will be needed to help facilitate the integration of these tests into the care of patients and workflow of clinicians across all specialties, the authors noted. In the future, Dr. Krantz anticipates every family could have the opportunity to ask for their infant’s genome to be sequenced as a newborn screening tool.
“When we look back at this period in medicine in 100 years, it’ll be seen as the genomic era of medicine,” Dr. Krantz said. “This testing not only enables us to find answers for families that until now have escaped our diagnostic ability — but also enables us to start to think about targeted treatments and preventative medicine.”
Generous support from the Roberts family has pioneered the RIMGC’s cutting-edge work to standardize CHOP’s approach to genetic and genomic testing. The Pediatrics paper presents how the RIMGC achieved cost-savings by centralizing services and avoiding dozens of individual clinical departments having to hire their own genetic counselors and specialized administrative and medical support staff. Building a community, constantly adapting to change, and teamwork and flexibility are some of the main factors contributing to the model’s accomplishments.
“We believe we have succeeded tremendously in this endeavor, especially since no other hospital had attempted a model like the one we established prior to the founding of the RIMGC,” Dr. Krantz said. “As this report outlines, even in a relatively short time, our Center has grown in response to clinical and research demands. We thought it was important to share what we’ve learned as more hospitals look to the model we’ve created to establish similar centers.”
As for Athan, he wakes up every morning with a smile on his face and excited for the day ahead, his mom said.
“Every day we learn something new about Athan’s abilities, and it amazes us,” Kristen said. “We continue to follow up with a few of the 16 departments, but each time we go, the list gets smaller and smaller. I would suggest to any parent that is looking for answers to think of genetic testing.”